- About ACNS
- Meetings
- Annual Meeting and Courses
- Principles of Clinical Neurophysiology Courses
- Claim CME: Past Meetings
- Endorsed Courses & Symposia
- Meetings & Programs Calendar
- Education
- Practice
- Research
- Advocacy
- Membership
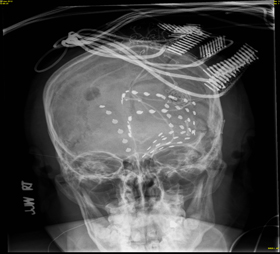
A 22 year old right-handed hispanic male was seen for evaluation of anxiety, spells, and seizures. His past medical history included a personal and family history of Tuberous Sclerosis Complex. Seizure onset was in early childhood manifest as “grand mal”. At puberty he began to develop “episodes” where he would scream and kick. These spells reoccurred daily to weekly. He did not respond to multiple antiepileptic drugs and anti-anxiety medication. Brain MRI demonstrated bilateral tubers without evidence of malignancy. EEG was normal. Subsequent video-EEG monitoring confirmed epileptic seizures with ictal EEG slightly lateralized to the left. Focal seizures began with a loud vocalization and growling evolving to side to side head movement while holding his head with bicycling movements for 30 seconds. An FDG PET revealed multi-focal hypometabolism greatest at a large left parietal tuber. SISCOM imaging was inconclusive as was alpha-methyl-trypophan PET. He was implanted with a broad multi-contact left hemispheric grid and strip array for iEEG (below) but had no iEEG changes in the first 10 seconds of behavioral seizure onset.
 |
 |
| A | B |
A second implanted electrode array was successfully.
 |
 |
| C | D |
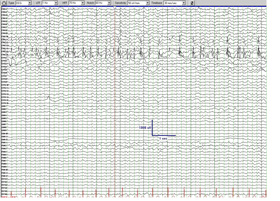
Figure A: Initial implant demonstrating multiple grid placement over the site of the left hemispheric including the largest brain tuber (A). Invasive EEG revealing no EEG changes in the first 10seonds following behavioral seizure onset (B). The second implantation of intracranial electrodes (C) abd the very focal iEEG (arrow) in the orbitofrontal grid noted in (D). Sensitivity 70 uv/mm; filters 0.1-100 Hz; timebase 30 mm/sec.; notched filter on.
Tuberous Sclerosis Complex (TSC) is often associated with drug-resistant epilepsy. Resective epilepsy surgery is fraught with difficulty when more than 1 seizure onset zone exists. Epilepsy surgery in TSC can be very successful when a single epileptogenic zone exists despite the presence of multiple intracranial tubers.1 Tonic seizures and moderate-severe mental retardation are risk factors for failed surgery. However a relation between multiple seizures types, early onset of seizures, multiple cortical tubers, and poor outcome have not been consistently noted despite the potential for multiple seizure onset zones.1 In our patient AMT PET was unfortunately unsuccessful in defining the active tuber among the many other tubers that were present. Intracranial EEG was initially non-localized with the original phase 2 evaluation. In patients with unlocalizable seizures, palliation by corpus callostomy might be considered.2 In our patient, a suspicion of a single SOZ and concern of misdirected iEEG was suggested by the lack of significant iEEG change during seizures despite the extensive implantation. This led to a second phase 2 dedicated to the left mesial and orbitofrontal cortex. In this case iEEG was highly localized (figure 1D) and a left frontal topectomy-lesionectomy has rendered him seizure free for >1 year.