- About ACNS
- Meetings
- Annual Meeting and Courses
- Principles of Clinical Neurophysiology Courses
- Claim CME: Past Meetings
- Meetings & Programs Calendar
- Endorsed Courses & Symposia
- Education
- Practice
- Research
- Advocacy
- Membership
Contributed by:
William O. Tatum IV, DO
Mayo Clinic Florida, Jacksonville, FL
A 21 year-old right-handed white female had recurrent generalized motor seizures (GMS) that were resistant to multiple antiseizure drugs. Seizures reoccurred on a monthly basis and she experienced repeated ASD intolerance and minor injury. Rare “petit mal seizures” were reported where she would abruptly stare and turn her head to the right with transient impairment in consciousness and post-ictal fatigue. Her “Grand mal” seizures would occur with a variable brief stare, impaired responsiveness, and head rotation to the right before evolving to a generalized motor seizure with bilateral tonic stiffening and clonic jerking for 1-2 minutes followed by brief post-ictal confusion and disorientation. She was a small, thin Caucasian female with a general physical and neurological examination that were normal.
A high-resolution 3-T brain MRI was normal. Interictal EEG demonstrated generalized bifrontally predominant generalized spike-and-slow waves (GSW) with a repetition rate of 3-Hz during wakefulness. Intermittent lateralization of GSW to the left was present during sleep. 3 typical seizures had a consistent semiology (at 2 institutions) with an ictal EEG demonstrating bilateral spike-wave at onset with clear left lateralization after 30 seconds in 1/3 seizures. An FDG PET reviewed weak left temporal hypometabolism. An MEG demonstrated a focal left superior-posterior temporal spike clustering.
She was strongly motivated to pursue aggressive intervention and was implanted with invasive electrodes for intracranial EEG (iEEG) seizure monitoring (figure 1). The results of her iEEG monitoring session are presented in figure 2.
What does her iEEG show that may influence treatment possibilities for her?

Figure 1: Brain cartoon demonstrating electrode contacts within a frontal and parietal 6 x 6 contact subdural grid, a left 1 x 6 contact superior temporal and frontopolar strip, and dual-sided inter-hermispheric strips approximating the anterior and posterior medial frontal lobe.
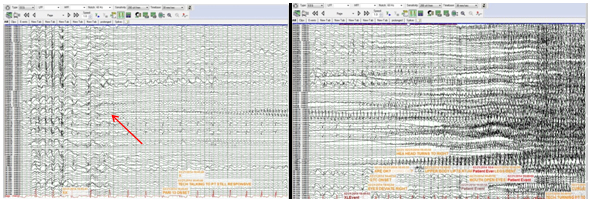
Figure 2: The intracranial EEG in our patient is displayed (a-d) and demonstrates;
The seizure seen during invasive EEG recording demonstrates a focal onset seizure. Normally, 3-Hz GSW in a young adult with recurrent GMS suggests one of the Genetic Generalized epilepsies (GGE). Furthermore GGE not uncommonly is associated with the presence of a clinical semiology with lateralized features. Patients with a 3 Hz GSW pattern on the interictal EEG may have this feature occur as an inherited trait independent of the phenotypic expression of clinical seizures. Additionally, 3-Hz GSW may rarely occur as a secondary bilateral synchronous discharge arising from a focal onset. This usually occurs with the presence of an electrographic “lead in” at the onset of GSW. It may also be associated with focal epilieptiform discharges and appears with a inter-spike interval less than 3-Hz. In secondary bilateral synchrony on the EEG, seizures typically have an onset that begins near the corpus callosum or is adjacent to the transcortical fibers that facilitate rapid propagation and the scalp EEG appearance of GSW.
The clues that our patient had localization-related epilepsy include the neurophysiological presence of a lateralized ictal scalp EEG and focal MEG cluster in addition to a consistently lateralizing semiology manifest as contralateral head deviation prior to seizure generalization. The uniqueness of this case lies in the exquisitely focal process of an extratemporal neocortical seizure onset as they usually demonstrate a regional iEEG onset that rapidly propagates. The ictal onset in our patient occurred at a single electrode in the left parietal grid despite the presence of 3-Hz GSW on scalp interictal EEG. The propagation that occurred over the subsequent 7-17 seconds was undetected on scalp EEG due to the low voltage associated with rhythmic ictal fast activity often associated with extratemporal neocortical generators. The extremely focal findings are in direct contradistinction to the generalized process suggested b interictal EEG.
Electrical cortical stimulation was performed for functional brain mapping subsequent to localizing the seizure onset zone by iEEG. The seizure onset zone was isolated within eloquent cortex (sensory). Treatment options included continued ASDs. She declined the modified Adkins diet as a personal choice with fears of weight loss and quality of life compromise. Surgery was suspected to produce a deficit and therefore neurostimulation was offered. Implantation of the responsive neurostimulator (RNS) was chosen in lieu of the vagus nerve stimulation due to the focality of seizure onset that was present. A discrete focal onset noted on iEEG suggests the potential to obtain a favorable outcome using RNS. Our case desmonstrates the continuum of generalized and focal seizures and illustrates the contrast between a non-localized scalp EEG seizure onset and a focal onset that may be encountered with iEEG despite scalp interical EEG revealing GSW.
References