- About ACNS
- Meetings
- Annual Meeting and Courses
- Principles of Clinical Neurophysiology Courses
- Claim CME: Past Meetings
- Meetings & Programs Calendar
- Endorsed Courses & Symposia
- Education
- Practice
- Research
- Advocacy
- Membership
Contributed by:
William O. Tatum IV, DO
The Mayo Clinic
Jacksonville, FL
A 25 year-old, right-handed female presented to clinic for “pass-out spells.” In her early teen years, she was noted to “faint” during heightened emotion. Episodes occurred initially every other month, then increased in frequency to become several times per week. Her symptoms occurred in the upright position with a feeling of gradually intensifying lightheadedness. Others would see her sway, become less responsive, and pale over a 2-3 minute duration. She had fallen during one of the episodes early when she was 15 years of age, prompting medical evaluation. She was seen by cardiology and diagnosed with neutrally-mediated syncope after a tilt-table test captured one of her events. Avoidance of stressful situations (behavioral modification), salt diet, fluids, and counter-pressure maneuvers were recommended. Holter monitor, echocardiogram, 12 lead EKG and cardiac exam were normal.
However, the “pass out spells” continued despite further cardiology management and over several years falls occurred repeatedly with injury becoming more frequent. They began to occur if she was sitting and even lying down at night when she would awaken with dizziness and confusion. Her examination was normal as was a brain MRI and routine scalp EEG by Neurology. An empiric trial of Levitiracetam was without apparent success. She was subsequently seen by the epilepsy service for evaluation and management.
What would you do now?
She was admitted for video-EEG monitoring. On day 1 after provocation from prolonged standing within a safety harness, an episode of lightheadedness was captured below.
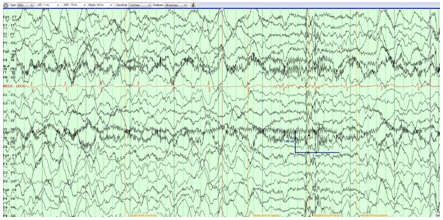
Figure 1
A 21 channel EEG obtained using an A-P longitudinal bipolar montage and a single channel of EKG obtained (parameters above). An event of severe postural lightheadedness was captured with the EEG demonstrating a diffusely slow background of 5-6 Hz with superimposed frequent bursts of 2 Hz frontally predominant delta activity.
What is her diagnosis?
Should she be discharged with a diagnosis of physiological nonepileptic events (PhysNEE) due to neurally-mediated syncope? With her nocturnal events she continued video-EEG with overnight recording where a different type of event was captured…
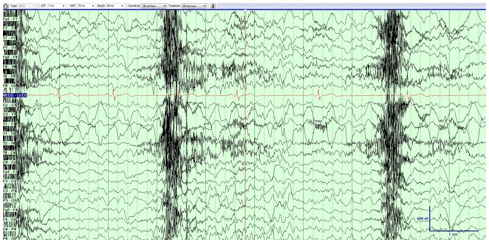
Figure 2
Continuous video-EEG during an episode of nocturnal “dizziness” captured prior to discharge. Note the left regional temporal rhythmic ictal delta during a subtle focal seizure without clinical signs or awareness mid-evolution following seizure onset.
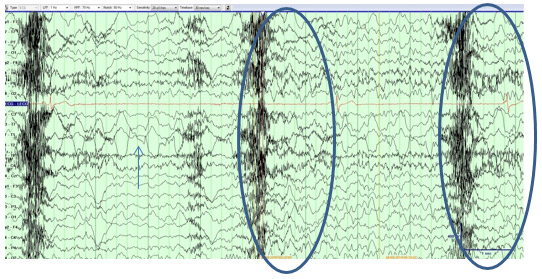
Figure 3
Sequential EEG obtained at the end of her event in figure 2. Note the focal seizure (arrow) and the severe ictal bradycardia on EKG with generalized theta and bursts of delta (ovals) in the last 5 seconds of the tracing (appearing similar to syncope in figure 1).
Syncope is the most common physiologic nonepileptic event (PhysNEE). Neurally-mediated syncope is the most common type affecting up to 40% of the general population. It occurs when a brief, transient self-limited loss of consciousness results from a global reduction of normal cerebral perfusion. When standing or sitting, the head is approximately 25-30 cm above the heart. Arrest of cerebral blood flow normally takes <10 seconds before consciousness becomes impaired and then lost. During this time the EEG becomes initially and increasingly is associated with progressive slower theta and delta frequencies that increase in amplitude (figure 1) and then start declining in amplitude until electrocerebral inactivity is reached as effective cerebral perfusion is compromised. EEG is usually not useful in syncope when the history clearly suggests it as the etiology. Electrocardiographic monitoring and echocardiography are more valuable tests than EEG. Head-up tilt table testing in our patient was diagnostic. Antiseizure drugs typically have no role.
However, a subtle electroclinical subtle focal seizure without awareness (SWA) was captured on day during overnight video-EEG (Figure 2). This was misidentified as a PhysNEE because of dizziness due to ictal bradycardia. Unless ASD taper and continuous EEG had been performed to capture the seizure, without awareness the presence of epilepsy would otherwise have evaded detection. Bradycardia and ictal asystole may rarely occur where a seizure has the secondary effect of transient cardiac arrest. Changes in seizure semiology may reflect syncope. In our patient the evolving non-positional quality, nocturnal predominance, and confusion suggested a 2nd process in addition syncope. In addition to ictal bradycardia, temporal lobe structures appear to be unique in predisposing to seizures without awareness. The loss of awareness may allow seizure to go unrecognized in 30% of epilepsy patients who are never aware of their seizures and only identifiable by clinical signs or by continuous EEG monitoring (1). Seizure awareness has a neuroanatomical foundation in the function of memory encoding and recall and therefore not unexpectedly occurs commonly in temporal lobe epilepsy (2). When seizures have a subtle semiology that is combined with patient unawareness, a definitive diagnosis of epilepsy may evade detection for years. Video-EEG is the means not only to diagnosis in this case but also critical in following the response to therapy. In our patient Leviteracetam was restarted and cardiology was consulted for evaluation of a pacemaker which may result in reduction of seizure-induced syncope and traumatic injuries due to falls associated with ictal bradydsyrhythmias (3).
References: