- About ACNS
- Meetings
- Education
- Practice
- Research
- Advocacy
- Membership
Contributed by:
Jonathan C. Edwards, MD and Ekrem Kutluay, MD
The Medical University of South Carolina
Charleston, SC
A 47-year-old African American female with a history of anemia secondary to fibroids was admitted to an outside hospital on for severe symptomatic anemia. Her hemoglobin at that time was 1.7. She received 4 units of PRBCs and underwent a workup including an attempted endometrial biopsy, which was unsuccessful She was discharged home on 04/23, but re-presented on 04/30 with acute onset headache, vision loss, and possible seizures. She was transferred to the Neuro ICU at the Medical University for further care.
MRI on arrival was consistent with PRES (Posterior Reversible Encephalopathy Syndrome). LTM EEG initially showed bilateral occipital periodic discharges (figure 1).
During the first day of EEG monitoring, the episode shown in figures 2 a-c was recorded.
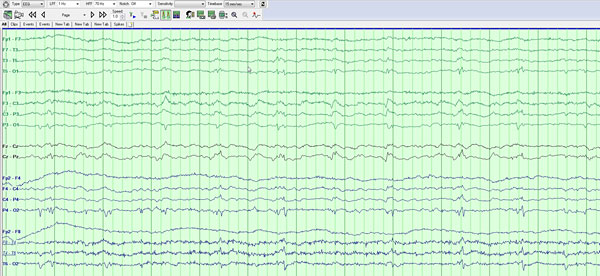
Figure 1: Baseline recording, showing bi-occipital periodic discharges
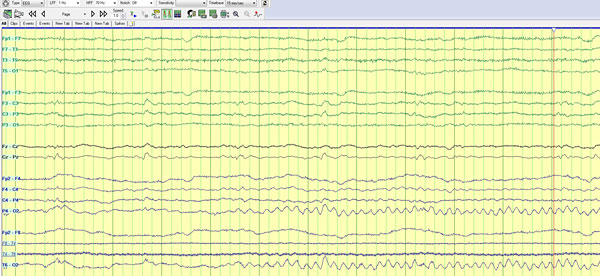
Figure 2a. Onset of rhythmic 5 hz actvity seen in the right occipital region.
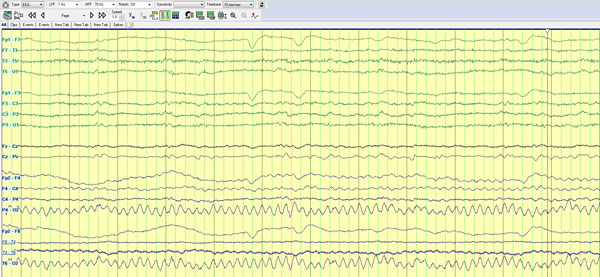
Figure 2b. 20 seconds later, spread to surrounding region. 6 hz
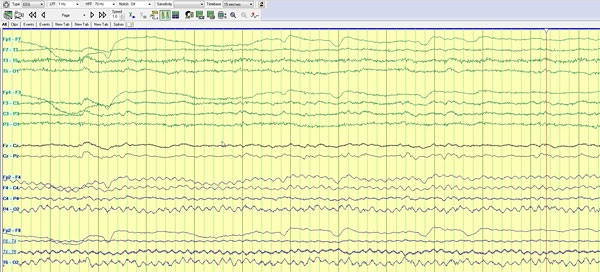
Figure 2c. 1 minute later, seen throughout right hemispheric electrodes
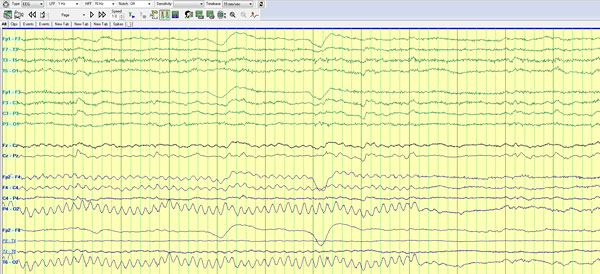
Figure 2d. 16 minutes later: end.
The activity seen on this record is an artifact generated by the “percussion” feature on the ICU bed. Percussion was used to treat the patient’s atelectasis noted on chest x-ray on arrival. This is an especially challenging artifact, because in begins in the same region as the posterior periodic discharges, in a patient with PRES. Additionally the activity evolves in frequency, amplitude and distribution. Such evolution would be very strongly suggestive of a non-convulsive seizure. The pattern was reproduced several times in the first few hours of recording.
Clues to the artifactual nature of this rhythm included the fact that while evolution was seen as described, the morphology of the theta rhythm remained the same through 14 minutes of the “event”. While there was apparent spread and a slight change in frequency noted over the first minute, the record was unchanged for the next 15 minutes. The neurophysiologist reviewed the video closely to look for a cause of possible artifact. At the end of the “event” the nurse can be seen walking to the bottom of the bed, and pressing a button on the bed’s digital control panel. The pressing of the button coincided with the termination of the finding. Further investigation in the ICU revealed that the bed function being used was “percussion”.
Continuous EEG monitoring in critically ill patients is a rapidly growing field, and is often the only reliable way to detect convulsive seizures and status epilepticus. However, an ICU is a complex environment with ample sources of artifact. Video is a powerful tool for sorting out some artifacts. A high level of suspicion for artifacts must be maintained, even in cases where “evolution” is seen.