- About ACNS
- Meetings
- Education
- Practice
- Research
- Advocacy
- Membership
Contributed by:
William O. Tatum IV, DO
The Mayo Clinic
Jacksonville, FL
A 63 year old right-handed male with treated hypertension, diabetes, and hyperlipidemia presented to the emergency department on Saturday evening after experiencing a witnessed “grand mal” seizure. CT disclosed a right frontal mass that was suspicious for a primary brain tumor. He remained encephalopathic and was able to verbalize but would drift off to sleep if left unattended. He was loaded with levetiracetam 1500 mg IV and continued on leviteracetam 500 mg IV b.i.d. Neurological examination revealed a new left hemiparesis though he was able to move against gravity. He was transferred to the NICU though remained somnolent improving over time to the point where he was awake and interactive. An EEG was ordered upon arrival to the NICU. He improved with resolution of his hemiparesis (Todd’s paralysis) and no further seizures apparent after treatment and by Sunday evening was discharged home. He mentioned that his "eyes were not quite right yet" at discharge.
His EEG was interpreted 1 hour after his departure and demonstrates the following.
What is your impression of this EEG and what would you?
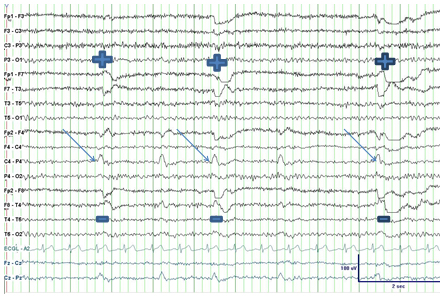
Figure 1
18 Channel EEG obtained with in an A-P longitudinal bipolar montage and a single channel of EKG demonstrating F4-C4 LPDs (arrows). Note the left horizontal eye movement artifact at the F7 electrode derivation identified by positive phase reversals (“+”) and corresponding negative phase reversals (“-“) at F8 providing electroclinical support for slow horizontal epileptic nystagmus.
The EEG demonstrated lateralized epileptiform discharges (LPDs) maximal at the right frontal-central electrode derivations (black arrows). The case lies on the interictal-ictal continuum where scalp EEG discharges appear interictal but there is an ictal correlate to the findings. LPDs may appear as spikes, sharp waves or even sharply contoured theta or delta complexes repeating at periodic (blue arrows) or semi-periodic intervals according to new terminology1. In this case LPDs were associated with left horizontal eye movements signified by the positive and negative symbols in the fronto-temporal electrode derivations. Extrapolating from this intermittent phenomenon and the clinical symptoms noted by the patient these LPDs would suggest a focal seizure.
Most LPDs are manifested on the EEG as epileptiform discharges (aka Periodic Epileptiform Discharges; PLEDs) that recur every 1-2 seconds occurring as bursts or runs. In this case the right fronto-central LPDs are commensurate with involuntary contralateral horizontal eye movements. This electroclinical constellation denotes the LPDs as a focal seizure (slow intermittent epileptic nystagmus) despite the periodicity of 0.5-1.0 Hz. When LPDs and appropriate clinical manifestations such as subtle eye movements or twitching appear continuously the finding of LPDs represent Focal (subtle) status epilepticus (aka Epilepsia Partialis Continua) on scalp EEG. When LPDs are intermixed with LPDs associated with focal rhythmic fast activity or rhythmic delta activity they may be referred to as “LPDs+” (aka PLEDs proper) and probably carry a greater risk of acute seizures and status epilepticus.2 Most electroencephalographers consider that there is a significant risk of ongoing seizure when frequencies exceed 1.5 – 2.0 Hz. Continuous EEG monitoring is helpful in identifying unrecognized seizures when mental status remains impaired after a seizure3.
LEV was a good choice in this case due to its’ favorable pharmacokinetics, concurrent condition and their drug treatments due to favorable pharmacokinetics and lack of drug-drug interactions. Structural lesions often predict a high risk for seizure recurrence as well as a poor response to treatment. He received additional LEV after this EEG and subsequently recovered without incident from his seizure though unfortunately was diagnosed with Glioblastoma multiforme on brain biopsy.
References