Featured Case - Summer 2020
Contributed by:
Roohi Katyal1, Chindo Mallum1, Masoom Desai2
1Resident, Department of Neurology; 2Assistant Professor, Department of Neurology, Division of Critical Care Neurology & Stroke, Division of Clinical Neurophysiology & Epilepsy, University of Oklahoma Health Sciences Center,
Oklahoma City, OK
Clinical Presentation
The patient is a 31-year-old woman with a history of multiple sclerosis, major depression, migraine, and spells of ‘fear-like sensation’ for five years. She presented with two episodes of involuntary shaking of all extremities presumed to be bilateral tonic-clonic seizures. Each episode had lasted approximately 4-5 minutes without return to her prior neurologic baseline between the events. Seizures stopped after she received 8 mg of intravenous lorazepam. Subsequently, she was intubated for airway protection and a loading dose of levetiracetam was administered.
Following extubation, she started having her typical episodes of ‘panic attack’, two to three episodes per hour, all during wakefulness. During these, the patient reported a “fear like sensation”; telemetry showed sinus tachycardia and tachypnea. These had been previously thought to be panic attacks /anxiety disorder and were being managed with paroxetine 20 mg daily on an outpatient basis.
Video-EEG monitoring was initiated to evaluate the etiology of these events. (Figures 1-3). During these episodes, she appeared scared and reached out to people to hold her hand. These lasted between 40-60 seconds each. There was no alteration of awareness during or after these events.
MRI brain with and without contrast with epilepsy protocol demonstrated the known burden of demyelinating lesions. Chronic demyelinating lesions were seen in bilateral occipital lobes, left > right, bilateral peri-atrial regions, bilateral frontal lobes and left midbrain. No new enhancing lesions were seen. Mesial temporal structures including hippocampal formations were normal.
 xxx
xxx
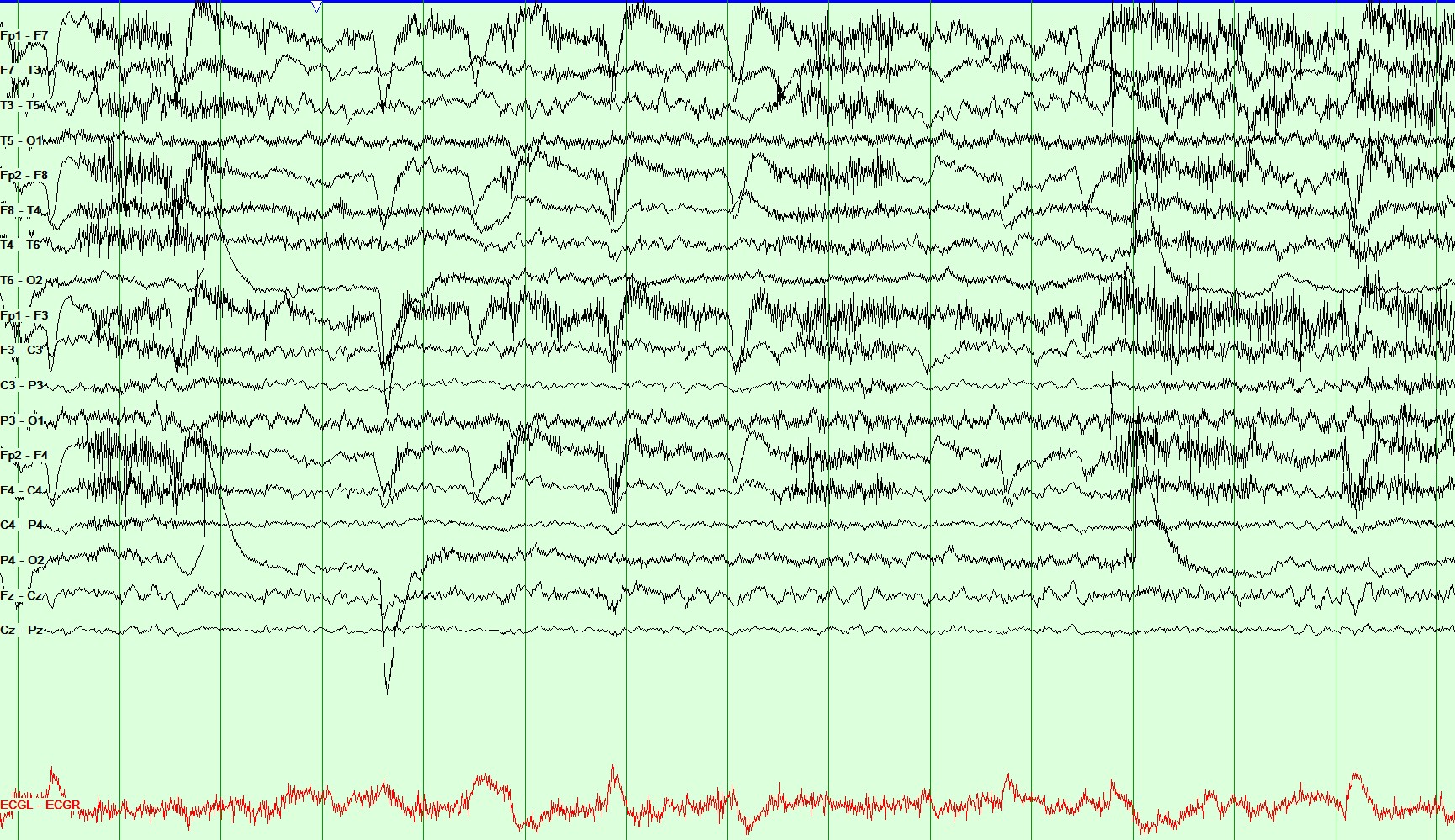
Figure 1: Longitudinal Bipolar Montage, Sensitivity: 20 microvolt/mm, HFF 70 Hz and LFF 1 Hz. During this EEG recording, the patient was tachycardic with a heart rate of up to 120 beats/min which was captured on the telemetry monitor (baseline 80-90 beats/min).
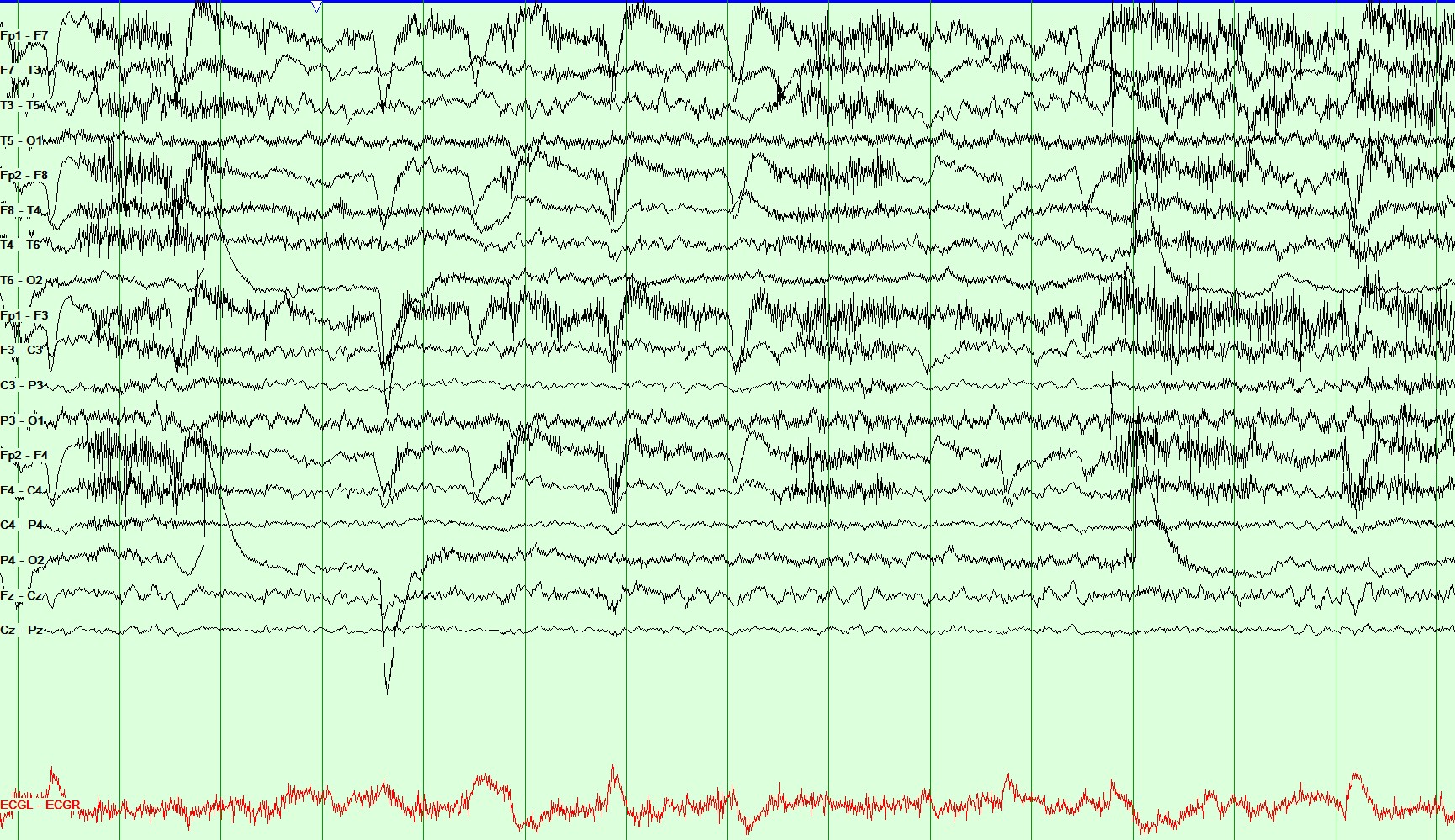
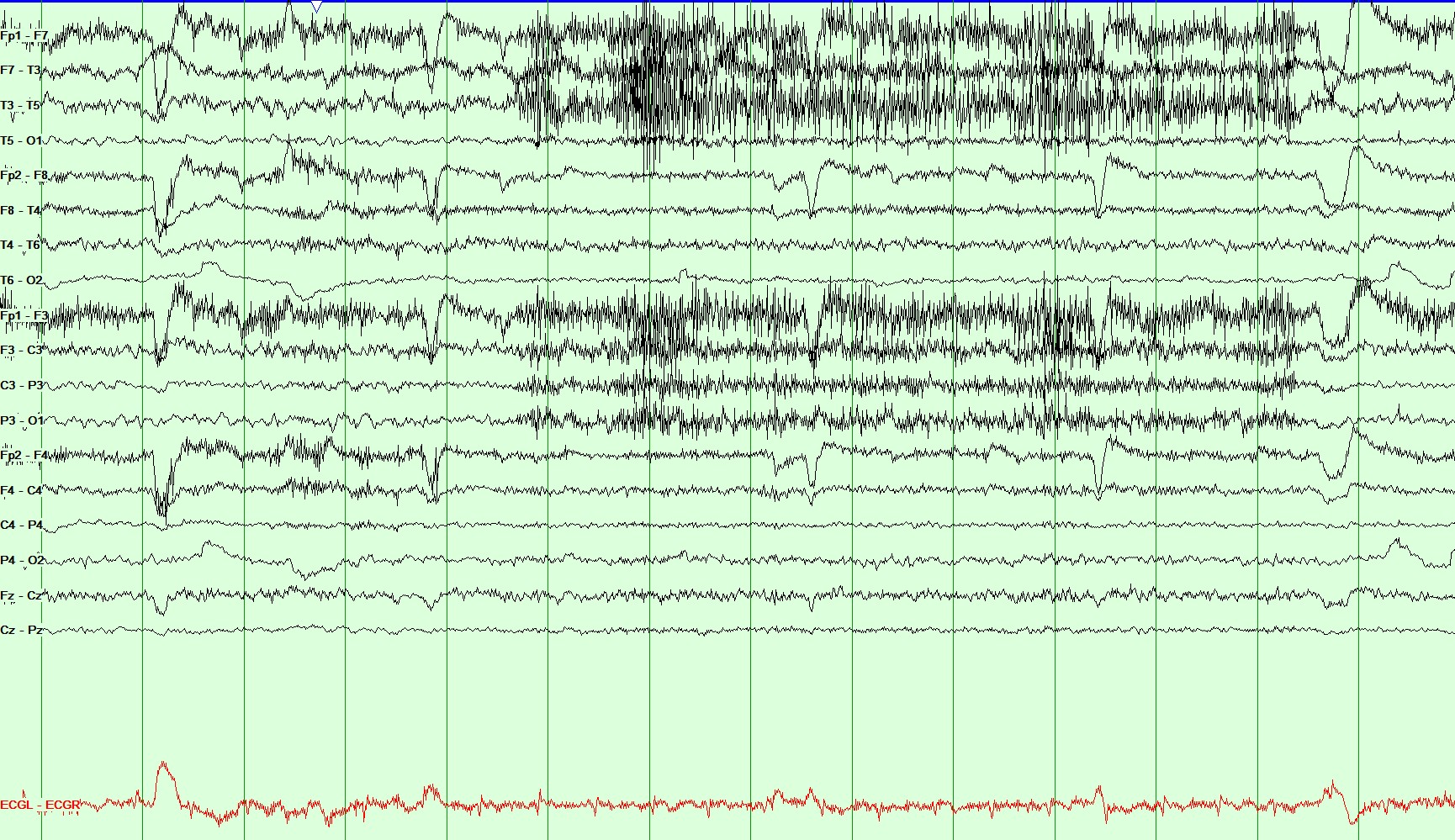
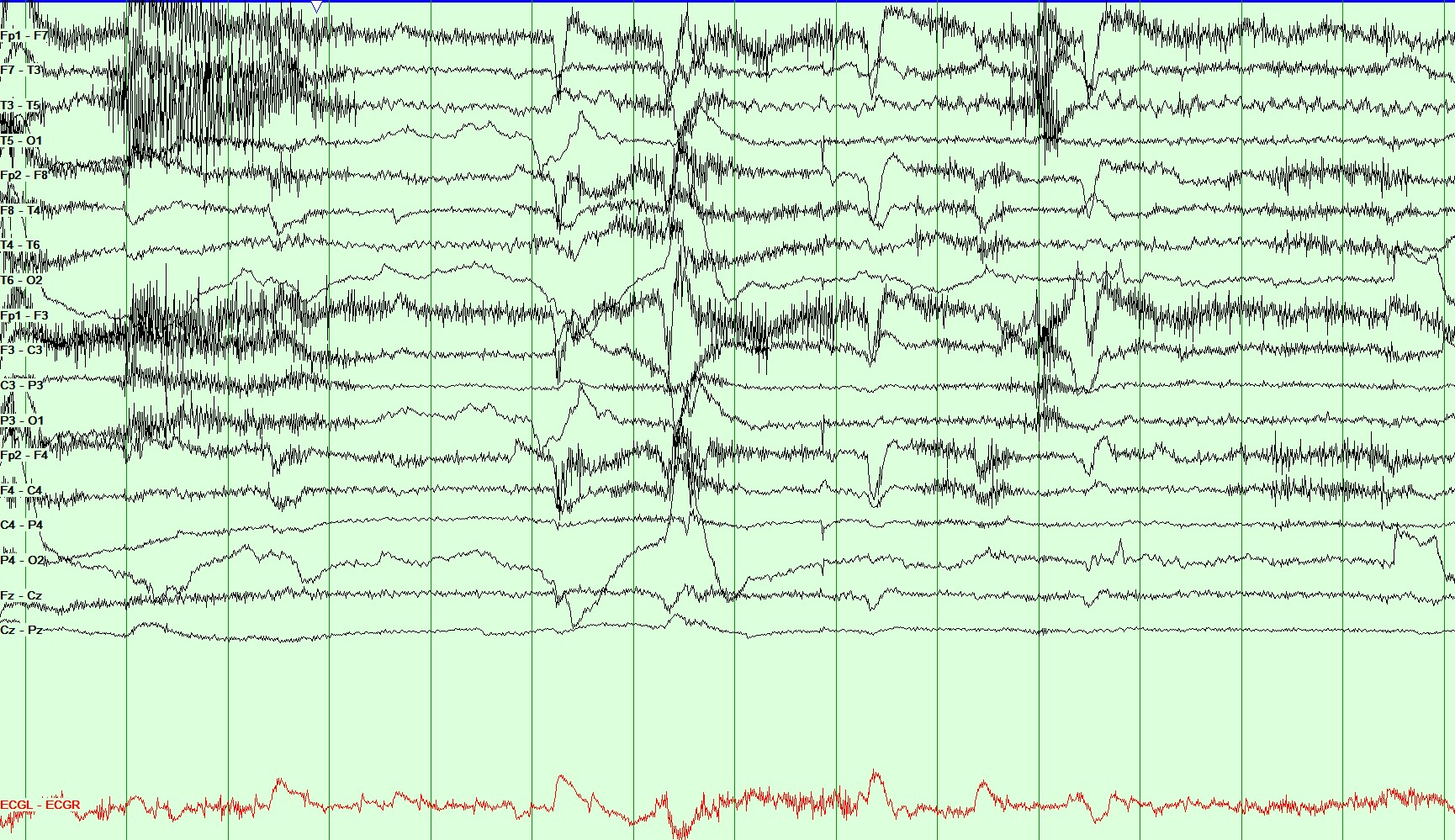
Figure 2: Longitudinal Bipolar Montage, Sensitivity: 20 microvolt/mm, HFF 70 Hz and LFF 1 Hz. This page demonstrates the continuation of the above spell. During this recording, the patient appears scared and reaches out for her hand to be held by the nurse at the bedside. She was tachypneic during this event with preserved awareness and continued to follow commands.
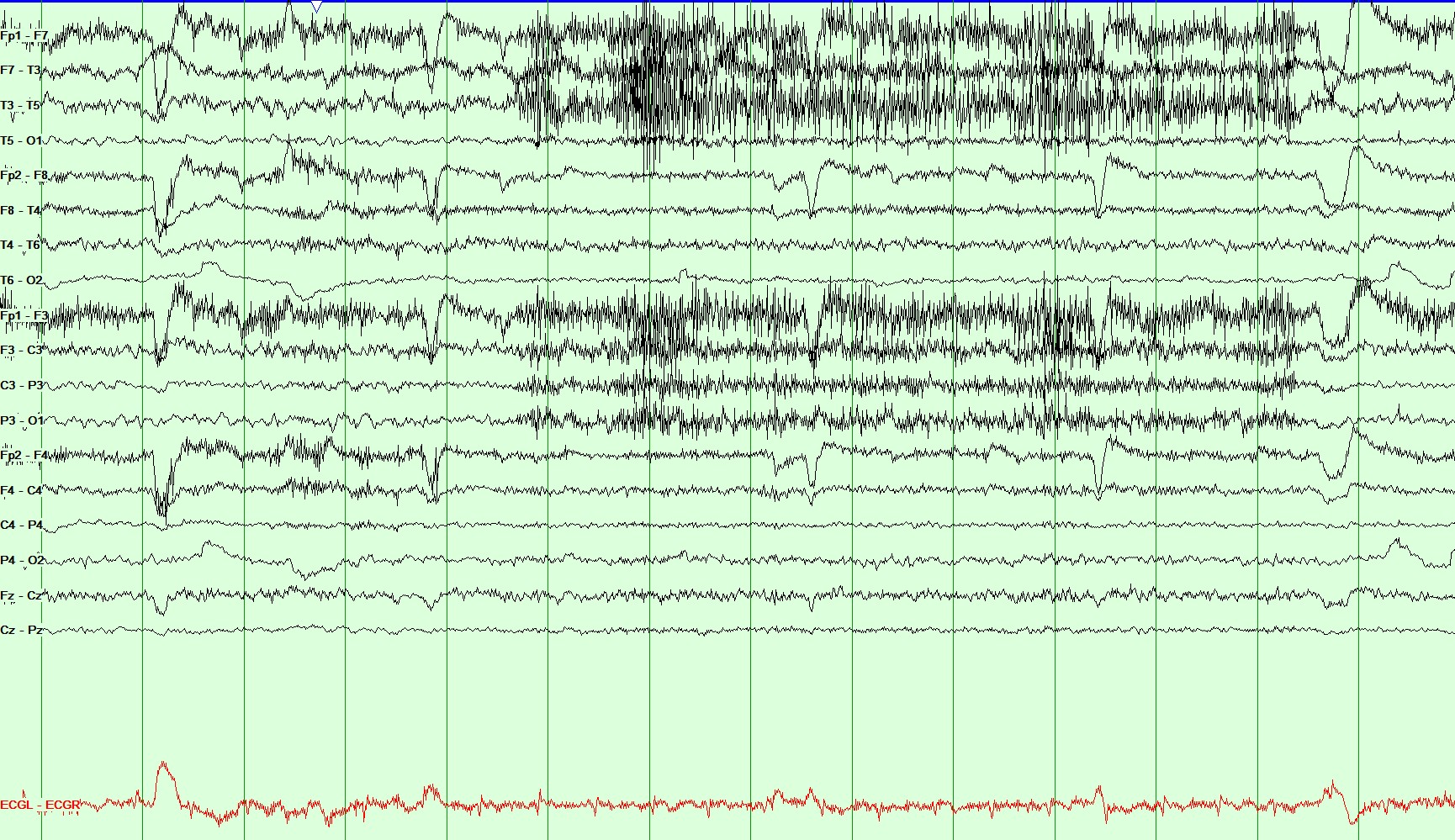
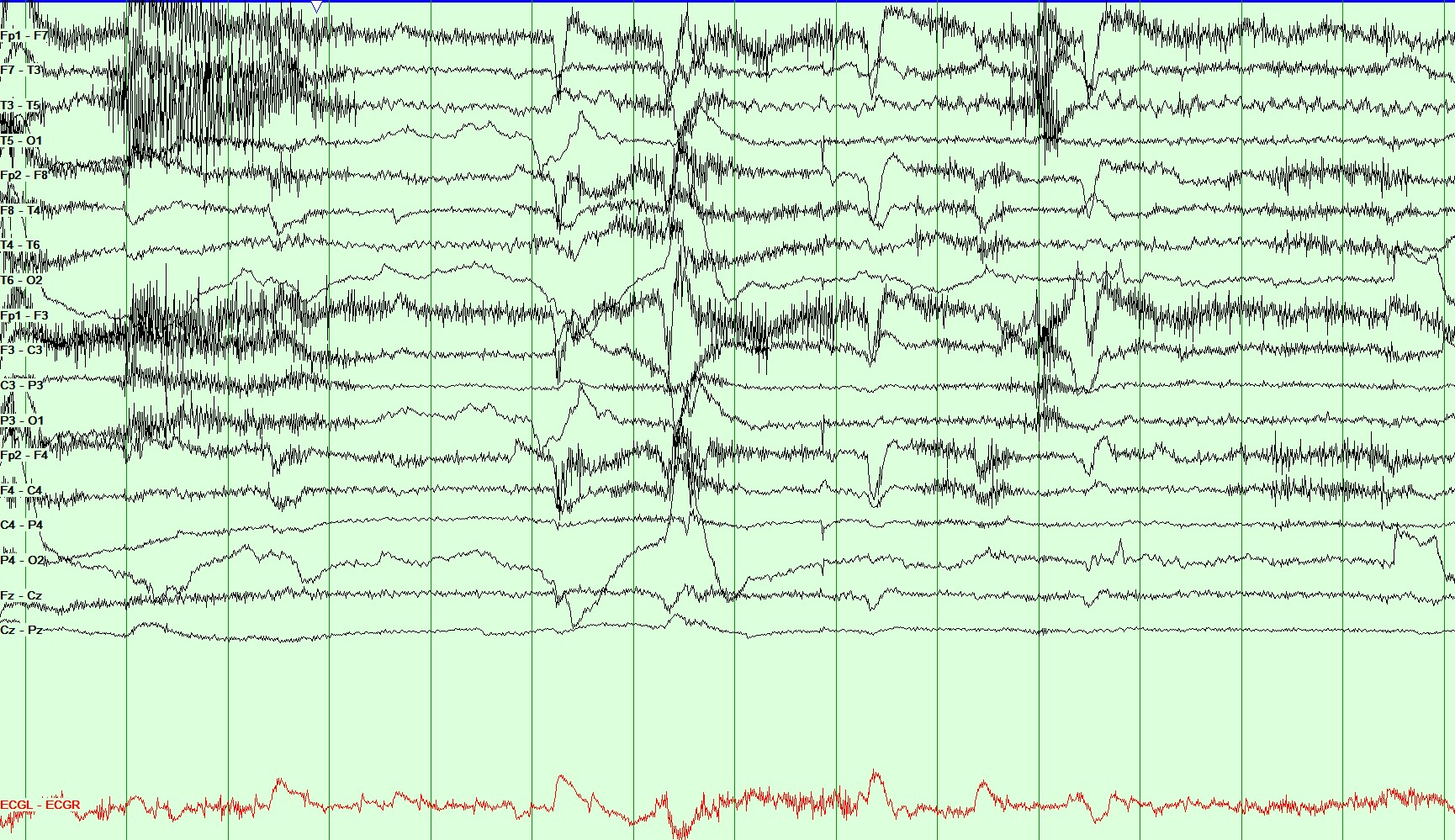
Figure 3: Longitudinal Bipolar Montage, Sensitivity: 20 microvolt/mm, HFF 70 Hz and LFF 1 Hz. This page demonstrates the last few seconds of the same spell. She continued to remain aware and tachycardic during this period.
Question 1: What conclusion can be drawn from this video-EEG and semiology description?
- Patient's clinical presentation and electrodiagnostic workup is consistent with the diagnosis of an acute panic attack
- Patient's clinical presentation and electrodiagnostic workup is consistent with the diagnosis of left temporal lobe epilepsy
- Patient’s clinical presentation and electrodiagnostic workup is consistent with psychogenic non-epileptic spells
- Patient's clinical presentation and electrodiagnostic workup is consistent with a subclinical seizure
Answer: (click here)
Correct answer: B. Patient's clinical presentation and electrodiagnostic workup is consistent with the diagnosis of left temporal lobe epilepsy
Question 2: What does the EEG recording in Figures 1 and 2 show?
- The EEG pattern is consistent with temporal lobe seizure.
- The EEG pattern is consistent with a benign variant (rhythmic mid-temporal theta-burst of drowsiness)
- The EEG pattern is consistent with intermittent temporally predominant small sharp spikes
Answer: (click here)
Correct answer: A. The EEG pattern is consistent with temporal lobe seizure
EEG shows temporal lobe seizure which is seen as rhythmic theta over the left temporal region at T3>F7, which evolves into higher amplitude and shows spread.
Question 3: How would you treat these episodes?
- Increase paroxetine in increments of 10 mg/day at an interval of >1 week up to a dose of 40 mg/day
- Start and continue maintenance anti-seizure medication
- Discharge home without anti-seizure medication and follow-up with outpatient psychiatry
- Discharge home without anti-seizure medication and a follow up elective epilepsy monitoring unit admission.
Answer: (click here)
Correct answer: B. Start and continue maintenance anti-seizure medication
Video-EEG over an hour recorded 3 habitual episodes, each lasting 40-60 seconds, for which the patient was loaded with additional anti-seizure medication and continued on maintenance doses. She reported one focal seizure with preserved awareness lasting ~30 seconds during neurology clinic follow-up after 1 week. Follow-up 3-weeks later revealed no further seizures.
Question 4: Which of the following is true when differentiating between ictal fear and panic attack?
- A panic attack will have symptoms of nausea, tachycardia, hot flashes, trembling, paresthesia, shortness of breath, sweating, which are not seen with ictal fear
- Ictal fear is always associated with alteration of consciousness and should not be confused with a panic attack
- Symptoms like loss of consciousness, duration of less than 2 min, nocturnal attacks, automatisms, déjà vu, lack of depressive symptoms and anticipatory anxiety are more often associated with ictal fear. Recording these episodes on video EEG is essential in most cases for final diagnosis 1-3
Answer: (click here)
Correct answer: C. Symptoms like loss of consciousness, duration of less than 2 min, nocturnal attacks, automatisms, déjà vu, lack of depressive symptoms and anticipatory anxiety are more often associated with ictal fear. Recording these episodes on video EEG is essential in most cases for final diagnosis 1-3
Symptoms of ictal fear have predominantly been associated with temporal lobe epilepsy3. A study by Feichtinger et al. emphasized the role of the amygdala, hippocampus and the parahippocampal gyrus in the mechanism of ictal fear5. The etiology of epilepsy in our patient remains unknown. She did not have any structural lesion in the temporal lobes on MRI brain. It is also important to note that focal aware seizures, unlike in our case, may not have an EEG corelate6. In such cases, spell description, emerging out of sleep and brief duration may help point towards the epileptic nature of these events. Additionally, patients with temporal lobe epilepsy may have associated physiological changes, for example, tachycardia, shortness of breath, etc.3 that may further aid in diagnosis especially in case of a negative scalp EEG.
A2: Correct answer: C. Acetazolamide
Patients with Hypokalemic Periodic Paralysis can be treated with acetazolamide, a potassium-sparing diuretic; those with CA-channel mutations are more likely to benefit than those with Na-channel mutations. Patients with Hypokalemic Periodic Paralysis should also avoid triggers, such as alcohol and carbohydrate-rich or salty meals. Acute attacks of weakness can be treated with oral potassium salts every 30 minutes until strength improves. Hypokalemic Periodic Paralysis may be allelic to malignant hyperthermia, hence patients undergoing surgery should be monitored accordingly
References
- N.N. Boutros, K. Gjini, J. Moran, H. Chugani, and S. Bowyer. Panic Versus Epilepsy: A Challenging Differential Diagnosis. Clinical EEG and Neuroscience. 44(4) (2013); 313-318.
- A.L. Johnson., A.C. McLeish, P.K. Shear & M. Privitera. Panic and epilepsy in adults: A systematic review. Epilepsy & Behavior. 85 (2018); 115–119.
- C. Brandt, M. Schoendienst, M. Trentowska, T.W. May, B. Pohlmann-Eden, B. Tuschen-Caffier, et al. Prevalence of anxiety disorders in patients with refractory focal epilepsy — a prospective clinic based survey. Epilepsy & Behavior. 17 (2010); 259-263.
 xxx
xxx