Featured Case - Winter 2020
Contributed by:
Amal Elhaj, MD
Clinical Neurophysiology & Epilepsy Fellow
Wake Forest Baptist Medical Center, Winston Salem, NC
Clinical Presentation
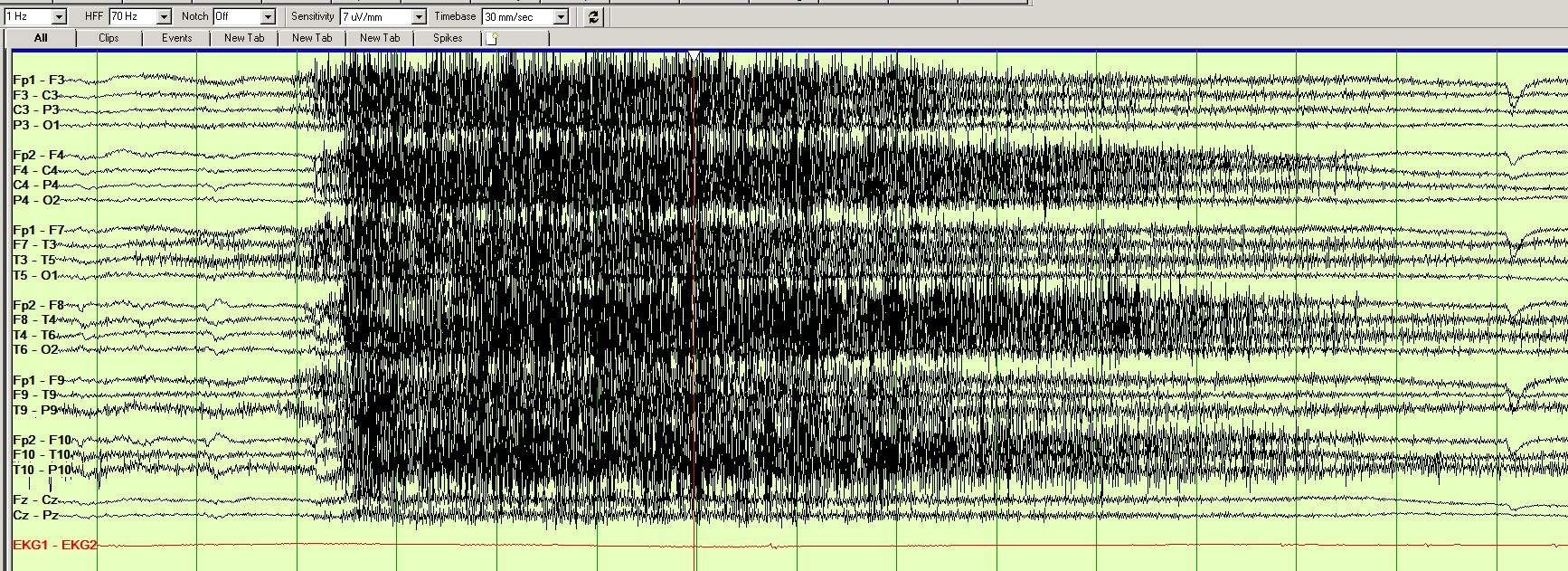
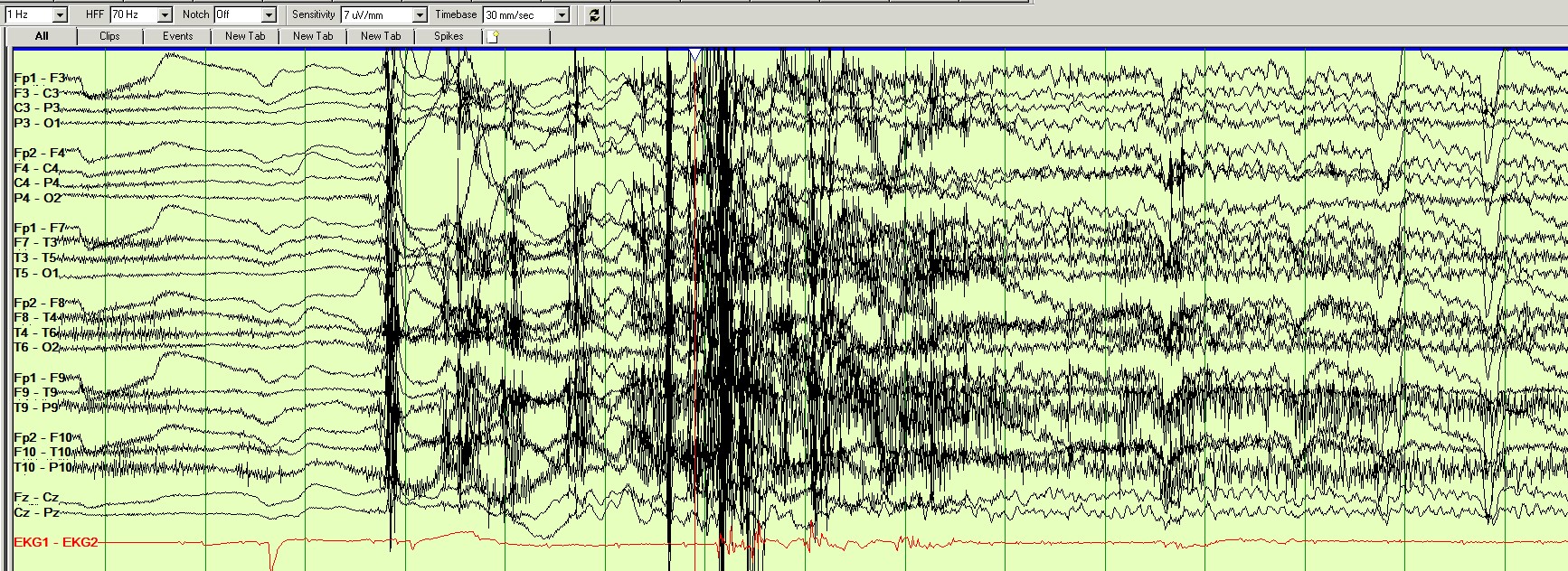
51 year old, right handed male with history of focal epilepsy with impaired awareness who was admitted to the EMU to further characterize and localize his seizures. He had 4 stereotyped seizures with similar EEG pattern starting with an aura of nausea, déjà vu and feeling of impending doom with 3 seizures progressing to impaired awareness, loss of consciousness, tonic posturing of upper extremities and myoclonic activity.
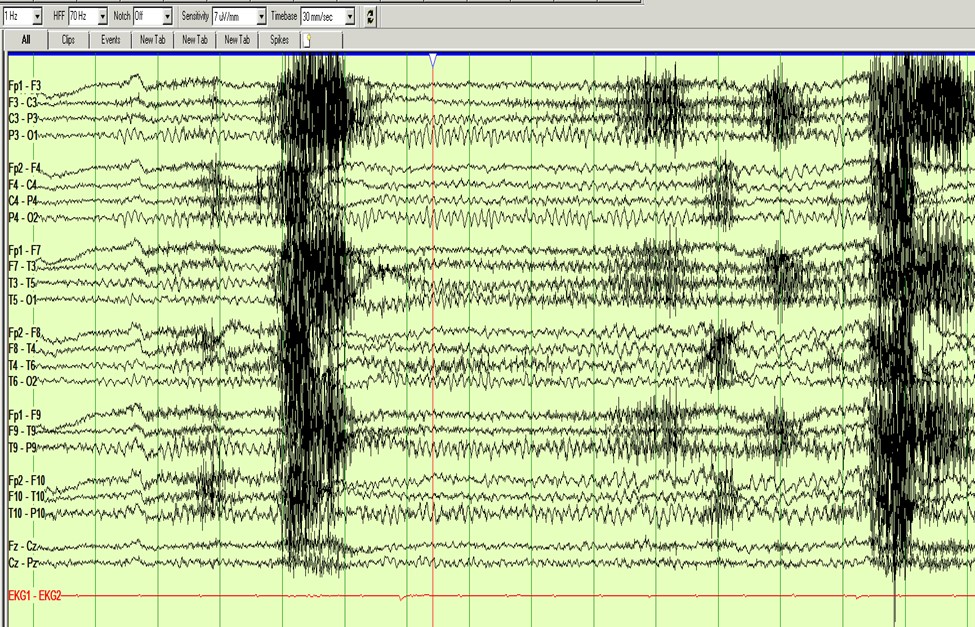
Question 1: Where does his seizure localize?
- Left temporal region
- Right temporal region
- Left frontal region
- Right occipital region
Answer: (click here)
Correct answer: B. Right temporal region
Patient’s EEG pattern localizes to the right temporal region. His semiology also supports the EEG findings localizing it to the temporal lobe.
Temporal lobe epilepsy is the most common cause of focal epilepsy. The semiological features include typical auras such as rising epigastric sensations, déjà vu, affective phenomena (fear or sadness), or experiential phenomena. Oroalimentary automatisms, contralateral dystonic, autonomic phenomena (change in heart rate and respirations), and prominent motor automatisms may be seen with temporal lobe epilepsy. Auditory, vestibular, complex visual hallucinations, aphasia and focal sensory-motor phenomena can also be present.
Review Article- Seizure Semiology: Value in Identifying Seizure Origin .Mohammed M.S. Jan, John P. Girvin.
The Canadian journal of neurological sciences, 2008 March
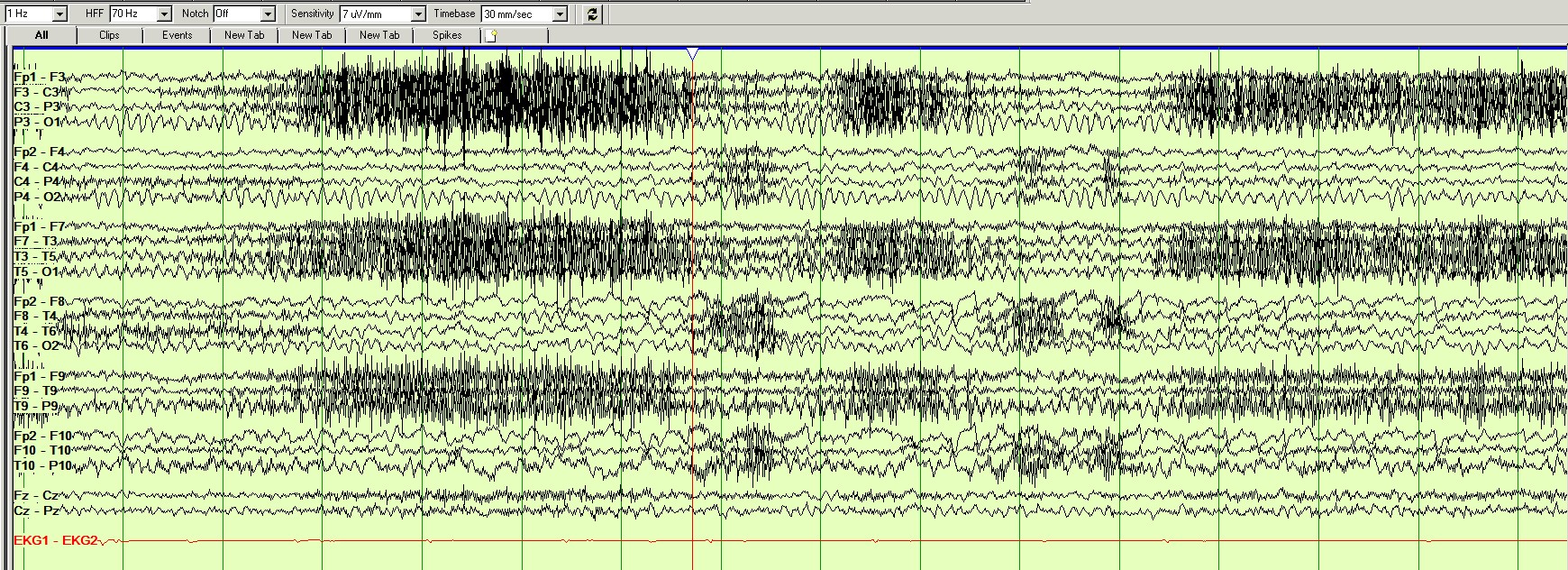
Question 2: How do you describe the EKG changes?
- Sinus tachycardia
- First degree heart block
- Asystole
Answer: (click here)
Correct answer: C. Asystole
Ictal asystole is defined as the absence of heart beat for a minimum of 3 s after the onset of seizure. The reported incidence is around 0.2–0.4% of patients. There are uncertainties in the pathophysiology, prognosis and treatment. The brain areas responsible of central autonomous system control are the insular cortex, amygdala, cingulated gyrus, hypothalamus and brainstem and prefrontal cortex, so an epileptic seizure affecting these areas is supposed to affect the heart rhythm. Most cases involve the temporal lobe, however seizures can be extra temporal or unknown. There is no clear evidence that ictal asystole increases the risk for SUDEP. Treatment has been controversial between optimizing AEDs only and placing a pacemaker as well. Pacemakers have shown to reduce the number of syncopal recurrences in refractory epilepsies but the indication remains unclear in non-refractory epilepsy and between symptomatic and asymptomatic groups.
Elsevier 2018: Ictal asystole: A condition between neurology and cardiology. Pepa Sánchez-Borque , Beatriz
González-Giráldez, Juan Benezet-Mazuecos, Angel Miracle, Julian Crosa, José M. Rubio.
Arrhythmia Unit, Cardiology Department, Fundación Jiménez Díaz – Quirón Salud, Madrid, Spain
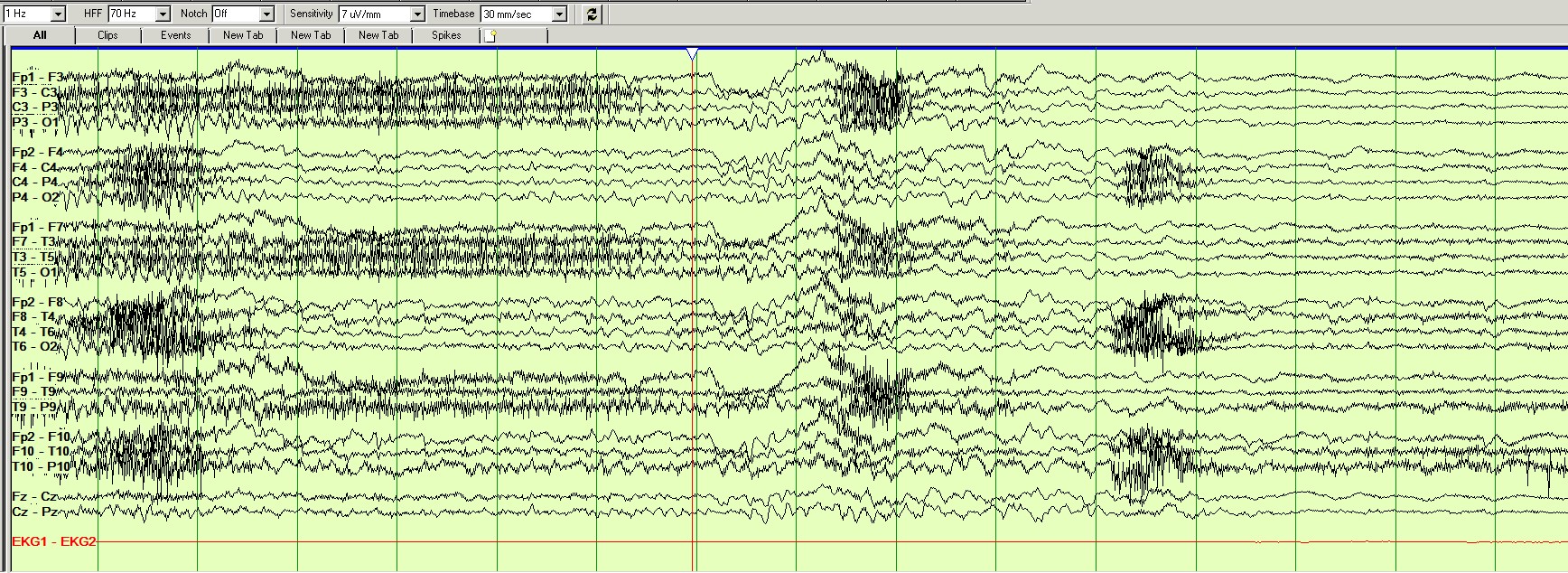
Question 3: How do you explain the diffuse slowing followed by diffuse attenuation on EEG after seizure onset and EKG changes?
- Decreased cerebral perfusion
- Increased cerebral perfusion
Answer: (click here)
Correct answer: A. Decreased cerebral perfusion
EEG slow-flat-slow is a classic marker of brain dysfunction during severe cerebral hypoperfusion and is associated with the presence of convulsive movements during syncope
Gastaut and Fischer-Williams, 1957; Ammirati et al., 1998; Sheldon et al., 1998; Martinez-Fernandez et al., 2008
References
- N.N. Boutros, K. Gjini, J. Moran, H. Chugani, and S. Bowyer. Panic Versus Epilepsy: A Challenging Differential Diagnosis. Clinical EEG and Neuroscience. 44(4) (2013); 313-318.
- A.L. Johnson., A.C. McLeish, P.K. Shear & M. Privitera. Panic and epilepsy in adults: A systematic review. Epilepsy & Behavior. 85 (2018); 115–119.
- C. Brandt, M. Schoendienst, M. Trentowska, T.W. May, B. Pohlmann-Eden, B. Tuschen-Caffier, et al. Prevalence of anxiety disorders in patients with refractory focal epilepsy — a prospective clinic based survey. Epilepsy & Behavior. 17 (2010); 259-263.